Describe the Managed Care Requirements for a Patient Referral
Patients managed care planthird party payer is identified. Take up to 10 business days to process your referral.
If patients have a managed care products HMO POS EPO their insurance does not allow them to self refer.

. Outline managed care requirements for patient referral 3. Generating Electronic Claims 1. We see only those patients with insurance referrals from a primary care physician PCP.
Specialty clinics are to ensure that referral had been obtained andor authorized by appropriate managed care planthird party payer. Describe the processes available for the verification of eligibility for services CASE STUDY all class members and determine the various types of insurance coverage that are represented by the students Have each student call to. Some referral ID are generated by your user.
But do not strictly rely on your computers spell-checker and grammar-checker. In your own words identify the steps for filing a third-party claim. Of the patient scheduling the appointment which directly influences the standard of care the patient receives.
Referrals are required for services considered to be specialty treatments. Outline managed care requirements for patient referral. Describe the electronic claim form.
Describe allowed charge contracted fee capitation and the formula for RBRVS. See the answer See the answer done loading. A verification of eligibility for services.
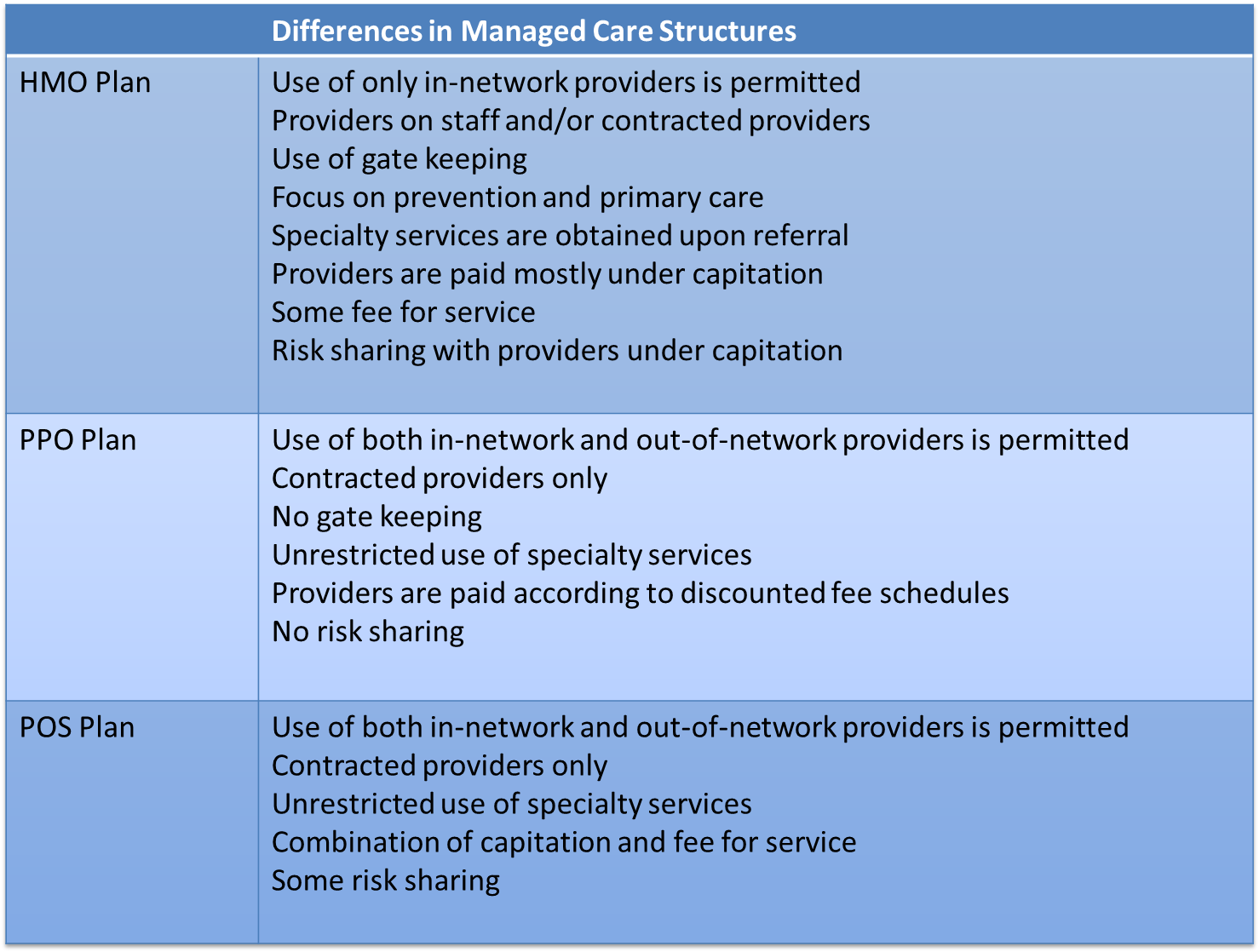
Managed Care is a health care delivery system organized to manage cost utilization and quality. Describe two ways electronic claims can be submitted. Managed care plans often have one or more of the following requirements.
In most health plans your primary care doctor manages your care. Medicaid managed care provides for the delivery of Medicaid health benefits and additional services through contracted arrangements between state Medicaid agencies and managed care organizations MCOs that accept a set per member per month capitation payment for these. Describe the managed care requirements for a patient referral.
Describe processes for verification of eligibility for services precertification and preauthorization. Outline the tasks performed to obtain the information required to produce an insurance claim. 111 148 as amended by the Health Care and Education Reconciliation Act of 2010 Pub.
The primary care office must coordinate document and approve all specialty visits. This means that you need a referral from your primary care doctor for most other medical servicesYou may also need prior approval for the service from your medical group or health planAn approval is. There is a co-pay obligation by the patient and.
Provide information on the patients current situation as well as other medical records test results and documents to avoid duplicate effort. It is you members ID for the community or program. Section 6401b of the Patient Protection and Affordable Care Act Pub.
Differentiate between fraud and abuse Procedural and Diagnostic Coding IXC 1. In the event that a patient has not been contacted a sending office can reassign the referral to a different provider and give feedback to the original receiving provider regarding access and patient follow-up. Record is reviewed to ensure appropriate documentation and signatures 3.
Describe the referral process for patients in a managed care product. The following is a brief explanation of specialty guidelines of the Access Dental Plan. Verification of eligibility for services b.
Patients are responsible for understanding their insurance coverage. Managed care transactions require an enormous amount of paperwork especially when the referral requests and authorizations never catch up to the claims submitted for the already provided services. The Primary Care Dentist requesting the referral must submit an Access specialty referral form.
A referral ID is a code that records the referral you generate so you can set compensated for it. 43 Staff Referral Responsibilities. Failure to do so indicates a lack of effort on your part and you can expect your grade to suffer accordingly.
Outline managed care requirements for patient referral patients seeking specialized care must first visit their assigned PCP to obtain a referral to a. Describe how to use the most current procedural coding system 2. 111152 collectively known as the ACA amended Section 1902 of the Social Security Act to add paragraphs a 77 and kk.
Submitting Claims to Third-Party Payers 1. Outline managed care requirements for patient referral VIIIC. Agree on the urgency of the referral how long the process might take how often to communicate and who will manage the patient during the referral timeframe.
A plan managed care index where 100 is a highly managed health plan measured the intensity of provider-oriented controls in a patients health plan based on the gatekeeping and lock-in provisions of the plans network the plans referral preauthorization requirements and whether the plan versus the provider was at financial risk. This problem has been solved. Define a patient-centered medical home PCMH 5.
You can obtain this form under Provider Forms. This results in a delay in payment to the provider and resubmitted claims as well as phone calls to the plan to resolve the problem. You must proofread your paper.
Describe how to use the most current procedural coding IXC. Outline managed care requirements for patient referral. Differentiate between fraud and abuse IXC.
4 Lis two different populations who would qualify for Medicaid 5 Outline managed care requirements for patient referral 6. Verification of eligibility for services b.

Managed Care Pharmacy 101 Amcp Org

Referral Form Template Word Lovely Sample Referral Form 10 Exam Digital Marketing Plan Template Digital Marketing Strategy Template Marketing Strategy Template
Comments
Post a Comment